For high-precision radiation therapy, it is necessary to carefully delineate targets and surrounding tissues to deliver high dose to the tumor while sparing critical anatomical structures. But accurately defining the target volume can be a challenge for clinicians. CT provides the Hounsfield Units (HU) required for dose calculations, but not enough of soft-tissue contrast. For this reason, there is a clear trend toward the increased use of MRI, with excellent soft-tissue contrast, for target delineation, monitoring and treatment adaptation.
The University Medical Center (UMC) Utrecht, a leading radiation therapy center in the Netherlands, has embraced MRI as imaging modality to enhance their radiation treatment planning. This is part of their mission to improve methods and provide excellent patient care. In a recent article in Philips’ FieldStrength MRI magazine, Dr. Marielle Philippens describes how UMC Utrecht has successfully made MRI a part of their standard clinical routine.
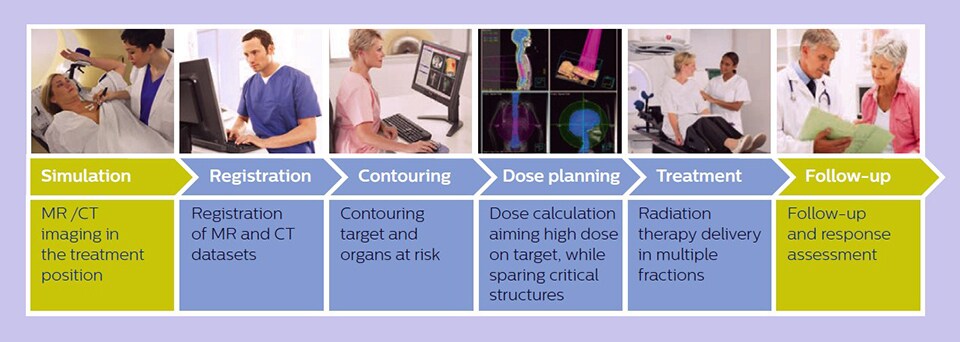
Simplified overview of MR imaging in radiation therapy workflow.
MR imaging in radiation therapy workflow
UMC Utrecht has deeply integrated MR into their clinical practice, using three Philips MR scanners for treatment planning. Every year, more than 1,300 patients undergo MR imaging for a variety of anatomies, such as the pelvis (including bladder, prostate, rectum and cervix), the brain, the esophagus, pancreas, the larynx and oropharynx, bone metastases and sarcomas. In addition, around 200 patients receive MR-guided brachytherapy in the prostate and cervix. UMC Utrecht developed and implemented dedicated imaging strategies for each anatomy to meet the different treatment planning requirements for MR.
For prostate, Dr. Philippens explains that all patients undergo an MRI exam – along with CT – before radiotherapy of the prostate to visualize the prostate and surrounding organs. “In addition to helping delineation of the prostate, MRI also helps in visualizing the lesions inside the prostate, which may not be possible in CT. When we can visualize intraprostatic lesions, the radiation therapist can then plan to boost them, giving a higher dose to those lesions instead of giving a uniform dose to the whole prostate, in the hope to better treat the patient and have less risk of recurrent tumors. However, this is not yet clinical routine.”
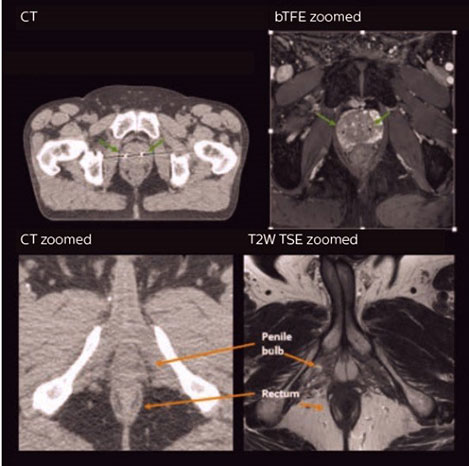
Clinical example: visualizing critical structures with MRI before prostate radiation therapy.*
A 63-year-old patient with prostate cancer, cT3bNxM, Gleason 7, underwent MRI on Ingenia 3.0T MR-RT before radiation therapy. Intraprostatic lesions are visible on the bTFE MR image, but not on the CT image.
MRI shows excellent soft-tissue contrast for the visualization of critical structures like the rectum and penile bulb. Fiducial markers (green arrows) are used in registration of MR images to CT, to transfer the MR-based delineations onto the CT image dataset.
Multi-disciplinary effort is the key to success
Introducing MRI into the treatment planning process starts with access to a dedicated MRI system with a flat tabletop and coil supports and coil setups specifically designed for radiation therapy MRI. Imaging patients in treatment position helps ensure that the delineated target volume matches the irradiated volume.
But, according to Dr Philippens, it is the team that makes the success. At UMC Utrecht, a clear, collaborative training plan has been set up to train the radiation therapy technologists on MRI. They need to know scan protocols and how to operate the MRI scanner, choose the coils and select the tabletops. Training and education of radiation oncologists helps achieve consensus and guidelines. It is also a good idea to involve radiologists, with their knowledge of MRI and tumor visualization and differentiation.
Dr Philippens: “I strongly believe it’s important to involve everyone in the process and contribute knowledge and experiences as a team.”
Research drives clinical practice
Prof Van Vulpen, Chairman of the Radiation Oncology Department at UMC Utrecht, sees great potential for MRI in radiation therapy. Not only for treatment planning, but also during and after treatment. As an example, the department is currently looking into how different MRI contrasts can be used to monitor treatment response for tumors in rectal cancer and esophageal cancer to help predict which patients will not need further surgery.
To learn more on how the close collaboration with Philips over the past 10 years has transformed how MRI is used in their clinical practice today, and how it can contribute to opening innovative new treatment pathways for MR-guided therapies in the future, watch the full interview with Prof Marco van Vulpen and Dr Nico van den Berg, MR Physicist.
For more information
Download the FieldStrength article about approaches for including MRI in radiation therapy planning, with more clinical cases and interviews from UMC Utrecht here
Or visit the Philips MR-RT product page
Written by:

Marieke van Grootel Product Marketing Manager MR Therapy