The Covid-19 pandemic spurred health systems and innovators alike to pivot and adapt quickly to respond to the crisis. One of the biggest leaps forward was that telehealth finally came to the forefront ensuring that specialists could access vital patient data and collaborate with each other regardless of location. Telehealth not only delivers a more convenient experience to staff and patients, but also extends the reach of care to those who may have trouble accessing it.
Here are ten telehealth examples that give a glimpse into the future of healthcare delivery.

1. Screening and engaging patients remotely before they enter a care facility Among the many examples of telehealth that were propelled during the pandemic, one that is likely to endure is online patient screening and engagement.
Since COVID-19 hit, hospitals and home care organizations have been using online questionnaires to triage and monitor suspected coronavirus patients, with call centers contacting high-risk patients for additional information before referring them to the appropriate care provider. As the pandemic abates, online screening and engagement tools will continue to see more widespread adoption – including increased convenience, a more engaged patient, and the potential to reduce hospital length of stay.

2. Welcoming patients to a care facility through digital front doors During the pandemic, leading radiology centers have used personalized text messages to remind patients of their upcoming exams, making them feel at ease by sharing links to safety protocols and other educational content. They have also virtualized their check-in processes, allowing patients to check in with a text message once they arrive at the hospital. Staff receive an automatic notification via the electronic health record system and can send a text message back once they are ready to see the patient.
This ‘virtual waiting room’ could very well become the new norm – allowing patients to enjoy a leisurely stroll or wait in the comfort of their car right until the start of their appointment.

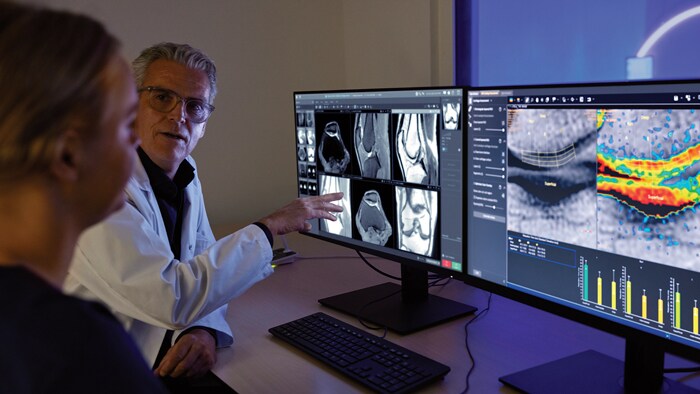
3. Supporting the acquisition of medical images remotely Like telehealth tools that connect patients to care providers, the use of provider-to-provider telehealth also skyrocketed over the past year, offering healthcare professionals new and innovative ways to collaborate even when they are far apart.
One such innovation in medical imaging comes from Philips - called the Radiology Operations Command Center - it enables expert imaging technologists to remotely train, guide, and assist less experienced or specialized colleagues in satellite locations. The power of this concept is that it allows for collaboration and over-the-shoulder support in real time, while the patient is on the scanner table. This help to ensure consistent image quality across sites, minimizing the need for unnecessary repeat scans. This model can also expand access to advanced imaging such as MR and CT at more locations, closer to where patients live, at more flexible hours - offering more convenience, and a better chance of getting timely diagnosis and treatment.

4. Bringing ultrasound expertise to the bedside with live remote collaboration Tele-ultrasound is another of many emerging examples of how telehealth can help to make expert knowledge more widely available throughout a health network – particularly in remote regions where specialized staff may be limited.
Although ultrasound technology is getting easier to operate, it still requires a relatively high level of manual skills, especially in more complex clinical cases. Using a live collaboration platform integrated into an ultrasound system, an experienced sonographer at an urban hospital can support a colleague at a remote site in performing the exam. A specialized doctor can use the same tele-ultrasound platform to provide instant reassurance to the patient and explain the exam findings from a distance, saving patients the stress of having to wait for their results.

5. Enabling interventional physicians to learn without having to leave their lab Interventional physicians, who perform image-guided minimally invasive procedures, have also started to explore the use of virtual collaboration platforms to continue providing peer-to-peer education.
In-depth knowledge of new and highly specialized interventional procedures can be limited to a small pool of physicians. Normally, these experts would be physically present in an interventional room to offer a less experienced user on-the-job training. Through virtual collaboration, they can look over their peer’s shoulder via webcams mounted on the ceiling of the interventional room. Similarly, technical experts – who know all the ins and outs of a specific treatment device or interventional system – can be called in for remote support before, during, and after procedures.

6. Assisting intensive care teams from afar Tele-ICUs are another great example of how telehealth can extend the line of sight of physicians to any hospital in the country – or even the world.
Led by an intensivist care team in a central monitoring facility that acts somewhat like an air traffic control center, tele-ICUs allow for patients to be monitored remotely and transitioned to the most appropriate care setting. Intensivists and nurses in the central hub are supported by high-definition cameras, telemetry, and advanced data visualization to assist their bedside colleagues, wherever they are located. Predictive analytics alerts care teams to early signs of patient deterioration, allowing them to intervene quickly when needed. During the pandemic, tele-ICUs have played a pivotal role in providing acute care support as ICUs were flooded with patients. Prior to the pandemic, tele-ICUs already demonstrated their value in addressing intensivist staff shortages. For example, through a cross-continental tele-ICU collaboration, critical care teams in Australia can keep a caring eye on patients in a US hospital to reduce the burden of traditional night shift work.

7. Keeping a caring eye on patients with wearable biosensors Where will remote patient monitoring go from here? Expect wearable biosensors to be a big part of the answer. Worn discreetly on the chest, these sensors can measure and transmit vital signs such as respiratory data and heart rate, as well as other patient data like posture and activity level.
Following the COVID-19 outbreak and the PPE shortages that initially accompanied it, hospitals have benefited greatly from using wearable biosensors to closely monitor patients on dedicated COVID-19 wards without exposing staff to unnecessary risks. Yet their potential application extends well beyond that – from low-acuity settings in the hospital all the way into people’s homes. For instance, in the long term, wearable biosensors could support remote monitoring of chronic diseases. The potential benefits include increased comfort for the patient, reduced cost of care, and an opportunity to act on patient deterioration earlier in order to prevent avoidable hospital readmissions.

8. Giving comfort to expecting moms through remote monitoring One large population set to benefit from new monitoring technologies are pregnant women, especially those at risk of complications. With many women worrying about the impact of COVID-19 infection on pregnancy1, the pandemic has highlighted the value of remote prenatal care.
Using a wireless pad and disposable electrode patches placed on the woman’s abdomen, caregivers can monitor vital signs of both mother and baby remotely to reduce unnecessary physical interactions.
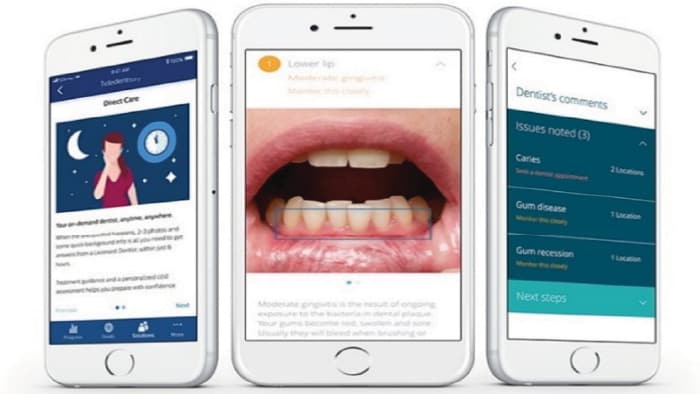
9. Promoting oral health through virtual dental visits Tele-dentistry cannot go unmentioned – because it offers exactly the sort of convenience and on-demand access that the modern health consumer desires - allowing patients to consult a licensed dentist via a mobile app, without having to leave their home or making an appointment. By sharing high-resolution photos of their teeth and flagging specific concerns, they can get a personalized assessment and practical advice for ongoing improvement of their oral health.
For dental professionals, many of whom switched to virtual consultations in the wake of the pandemic, tele-dentistry offers a way of keeping in touch with patients in between visits, allowing them to monitor progression of oral health conditions such as gum disease or to follow up on treatment remotely.

10. Offering easy access to telehealth Despite the clear potential of these and other telehealth examples to improve access to care regardless of where patients live, the pandemic has also sparked concerns that large parts of the population may be left behind because they lack access to a reliable internet connection2.
This has brought to the fore the importance of ICT and telecommunication in healthcare to allow for faster transmission of information, as well as digitization of complex data, which will accelerate efficient interaction between healthcare professionals and patients. At Philips, for instance, we partner with leading telecom players across the globe to realize telehealth’s full potential for the future. Most recently, we signed a memorandum of understanding with du, from Emirates Integrated Telecommunications Company (EITC), to collaboratively transform healthcare in the United Arab Emirates (UAE), as well as partnered with The Saudi Telecom Company (STC), the largest telecom operator in the Middle East, to rollout telehealth solutions powered by Artificial Intelligence. It’s a clear sign of the future to come: one in which patients will be able to connect with their providers anytime and anywhere, through a smart combination of home-based monitoring, telehealth visits, and physical access points close to where patients live.
1 Nanjundaswamy MH, Shiva L, Desai G, et al. (2020). COVID-19-related anxiety and concerns expressed by pregnant and postpartum women-a survey among obstetricians. Arch Womens Ment Health. 23(6):787-790. https://doi:10.1007/s00737-020-01060-w 2 Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: How COVID-19's telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83(5):e345-e346. https://doi:10.1016/j.jaad.2020.07.043
Topics
Author